It's not uncommon for older female patients to present to the gynecologist complaining of acute or chronic pelvic or abdominal pain. In many cases, pain can be attributed to problems affecting one or both ovaries. Arriving at a definitive diagnosis concerning postmenopausal ovarian pain, however, requires a careful and precise approach.
It isn't enough to simply ask a patient about their symptoms; instead, physicians must systematically rule out potential causes of ovarian pain. By using a comprehensive method of checking for and eliminating causes, you can help postmenopausal patients with ovarian pain begin treatment for the underlying problem as soon as possible.
Potential Causes of Postmenopausal Ovarian Pain
Ovarian pain can be attributed to several possible causes, including:
- Endometriosis: While rare after menopause, endometriosis may occur as a result of hormone replacement therapy and may cause significant pain.
- Ovarian cysts: While the incidence is low, older women may be affected by ovarian cysts. Studies suggest a wide range — 2.5 to 14 percent, according to the World Journal of Obstetrics and Gynecology — in the prevalence of ovarian cysts in postmenopausal women.
- Ovarian cancer: In some cases, pain may be directly correlated to ovarian cancer. Women over 60 years old are at a higher risk for this type of cancer.
- Pelvic adhesions: Adhesions may form around any part of the female reproductive tract, including the ovaries. Adhesions may be particularly painful depending on the size of the scar tissue.
Evaluating Postmenopausal Ovarian Pain
While there isn't any one method of assessing your patient for causes of ovarian pain, you can still use a systematic approach to thoroughly evaluate each patient:
- History: Each assessment should begin with a discussion of the patient's medical history, specifically focused on abdominal or gynecological conditions and surgeries. To evaluate the nature of your patient's pain, ask about its location, intensity, timing, duration and any factors affecting it. You should also ask about your patient's social history, including family health history and a discussion of sexually transmitted infections (STIs).
- Physical examination: A whole body physical examination is necessary to help rule out other causes of pain. Patients with postmenopausal ovarian pain should undergo a thorough pelvic examination in addition to a standard exam.
- Laboratory testing: Blood and urine should be collected for evaluation in a laboratory. In addition to all standard blood tests, serum CA 125 results may be used to indicate possible malignancy. Any abnormal results require further follow-up and should not be used in isolation to make a diagnosis.
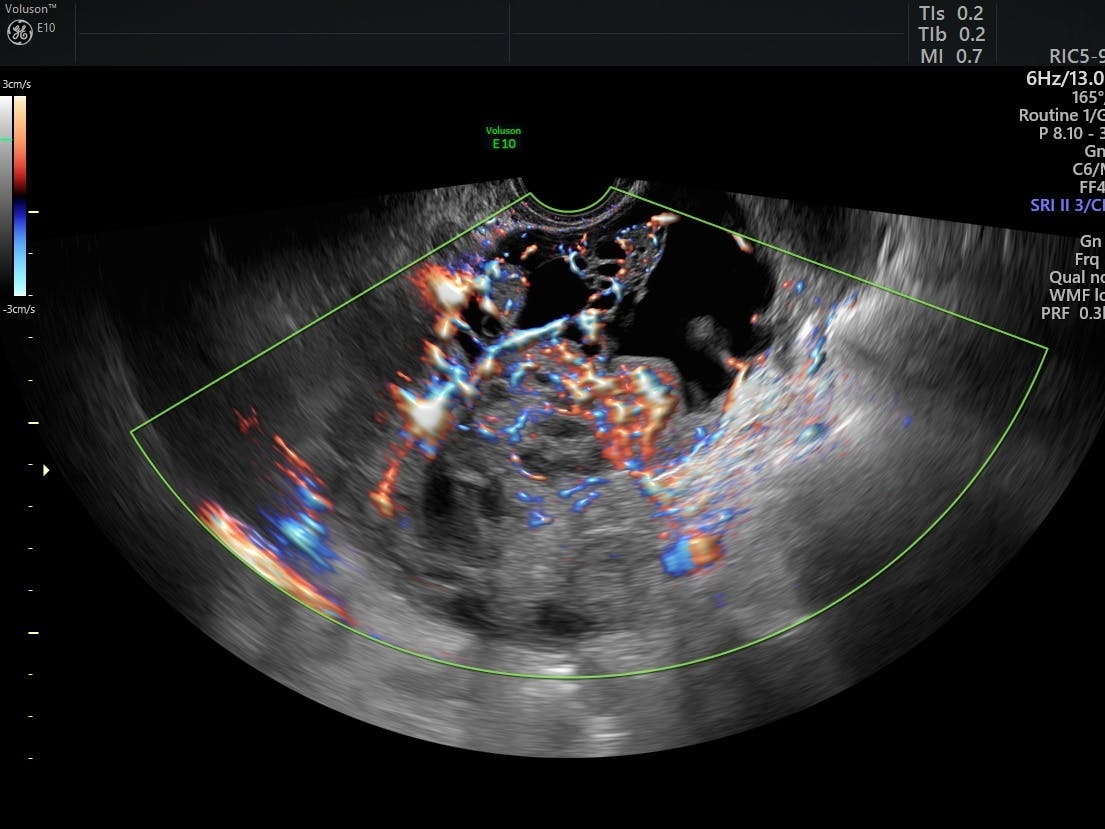
- Imaging tests: Transvaginal ultrasound provides invaluable information about your patient's unique anatomy. This imaging modality may be used to detect ovarian masses or assess the patient's entire pelvic floor. Results from transvaginal ultrasound may be used in combination with additional imaging tests, including CT and MRI.
Determining the cause of postmenopausal ovarian pain presents a unique challenge to gynecologists. Systematically identifying the factors causing pain will help you develop the best treatment plan for managing your patient's symptoms. Working together with your patient to complete a detailed whole-body examination is key to arriving at a diagnosis quickly.