Here are some common concerns that OB-GYNs might need to address when treating patients with heavy bleeding, PCOS, and other forms of difficult menstruation.
For most menstruating people, periods amount to a few inconvenient and occasionally unpleasant days each month. But for some patients, heavy, abnormal menstruation can disrupt daily activities and even affect quality of life. Here are some common questions and concerns that OB-GYNs might need to address when treating patients with difficult menstruation, and suggestions for how to provide care that is both empathetic and clinically appropriate.
- What do clinicians need to know when prescribing tranexamic acid for heavy periods? Excessive menstrual bleeding, or menorrhagia, is a common complaint that adversely affects a patient's quality of life. Tranexamic acid—an antifibrinolytic that slows the breakdown of blood clots—can be an effective, non-invasive way to treat menorrhagia caused by a hormone imbalance. Before prescribing tranexamic acid or hormonal contraception, clinicians should conduct a thorough pelvic exam with ultrasound to rule out any concerning pathologies that might account for difficult menstruation.
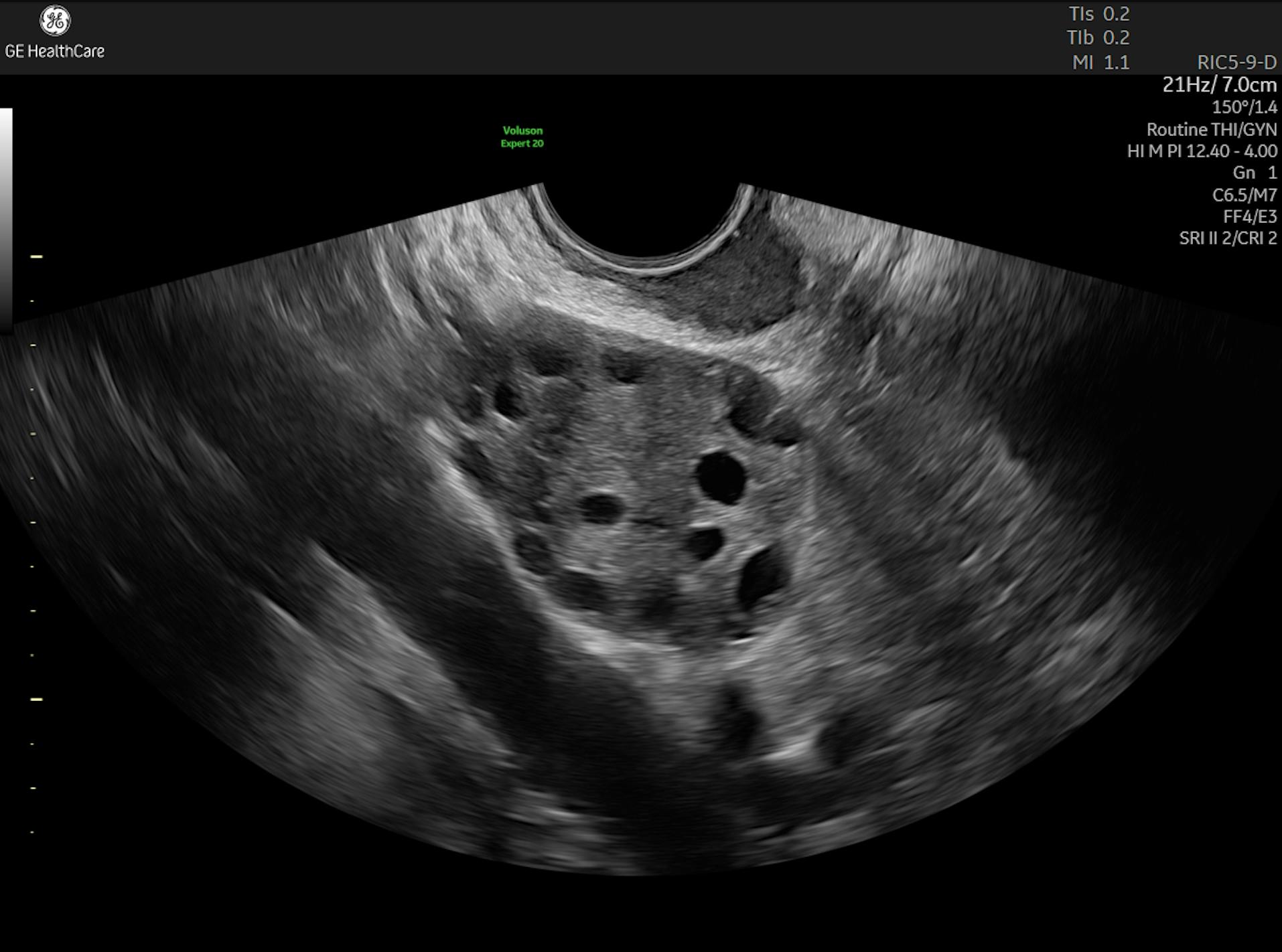
- How are anovulatory cycles managed in adolescent patients? Anovulatory cycles—menstruation without ovulation—is fairly common for young girls during the first year after menarche and can lead to prolonged, excessive bleeding. Anovulation is typically caused by immaturity of the hypothalamic-pituitary-ovarian axis. If symptoms persist for more than a year, patients might need to be evaluated for other causes, such as polycystic ovarian syndrome (PCOS), which can be identified via pelvic ultrasound. Clinicians should monitor adolescents with heavy bleeding for anemia. They might also consider dietary changes and hormone therapy to manage symptoms of anovulation.
- How do clinicians assess abnormal uterine bleeding in adolescents? When assessing adolescents with abnormal uterine bleeding (AUB), clinicians work with the patient to map out a thorough menstruation history. They might also screen for sexually transmitted infections, pregnancy, and thyroid disorders. Then they conduct a physical exam and do initial lab work, including a finger-stick hemoglobin test to look for underlying clotting issues. Some patients with difficult menstruation might also benefit from a transabdominal ultrasound to look for structural uterine abnormalities or possible endocrine disorders such as PCOS.
- How can clinicians address common concerns for patients who start menstruating earlier than expected? The average age at first menstruation has steadily dropped over the past century, from 13.3 years old in 1920 to 11.9 years old in 2020. However, early signs of puberty may happen as early as age eight. It's important for clinicians to know how to address patient and caregiver concerns about early menstruation, including reassuring them that early menstruation—and irregular menstruation during the first few months—is normal. Clinicians should also know how to provide sensitive, age-appropriate care that balances the need for clinical information gathering with the need to put young patients and their concerned parents at ease.
- How do COVID vaccines affect menstrual cycles? Current research has not established a clear connection between COVID-19 vaccines and menstrual changes, but some vaccine recipients report having one or two unusually heavy, painful periods after the second dose. OB-GYNs should be prepared to discuss patient concerns about the vaccine's effect on menstruation and reassure them that a brief vaccine-related disruption is unlikely to cause any long-term harm or fertility issues. Patients experiencing repeated abnormal cycles or heavy bleeding should be evaluated for endometriosis or fibroids.
- How do clinicians diagnose and treat PCOS in teens? PCOS can be challenging to identify in adolescents because the symptoms—menstrual irregularity and heavy periods—can also be a normal part of puberty. The current best practice for diagnosing PCOS in teens involves bloodwork and an ultrasound exam. Maintaining a healthy weight may help to mitigate symptoms, so OB-GYNs might refer patients to a nutritionist or general practitioner for assistance managing their blood glucose and insulin levels. These patients might also be prescribed oral contraceptives to correct hormonal imbalances and/or metformin to support healthy insulin levels.
Periods are an unavoidable part of life for half the population—and while periods are normal, heavy bleeding and irregular cycles are not. Patients experiencing difficult menstruation don't need to suffer in silence. They should be evaluated by clinicians who know how to deliver proper care and address concerns in a sensitive, age-appropriate way that puts patients at ease while also meeting their needs.