The nuchal translucency (NT) ultrasound is a milestone screening for most pregnant patients. Still, patients typically undergo tests and screenings at the recommendation of their healthcare provider without really understanding how valuable the exam can be.
The goal of this article is to break down this fetal ultrasound test into understandable terminology and explain what it means for potential parents and their future newborns.
What Is Nuchal Translucency?
First, what is NT? NT is a fluid-filled area seen on ultrasound behind the neck of a developing fetus. In the image below, it is the anechoic (black) stripe of fluid between the two yellow cross calipers; at its maximal thickness, the NT here measures 1.54 mm.
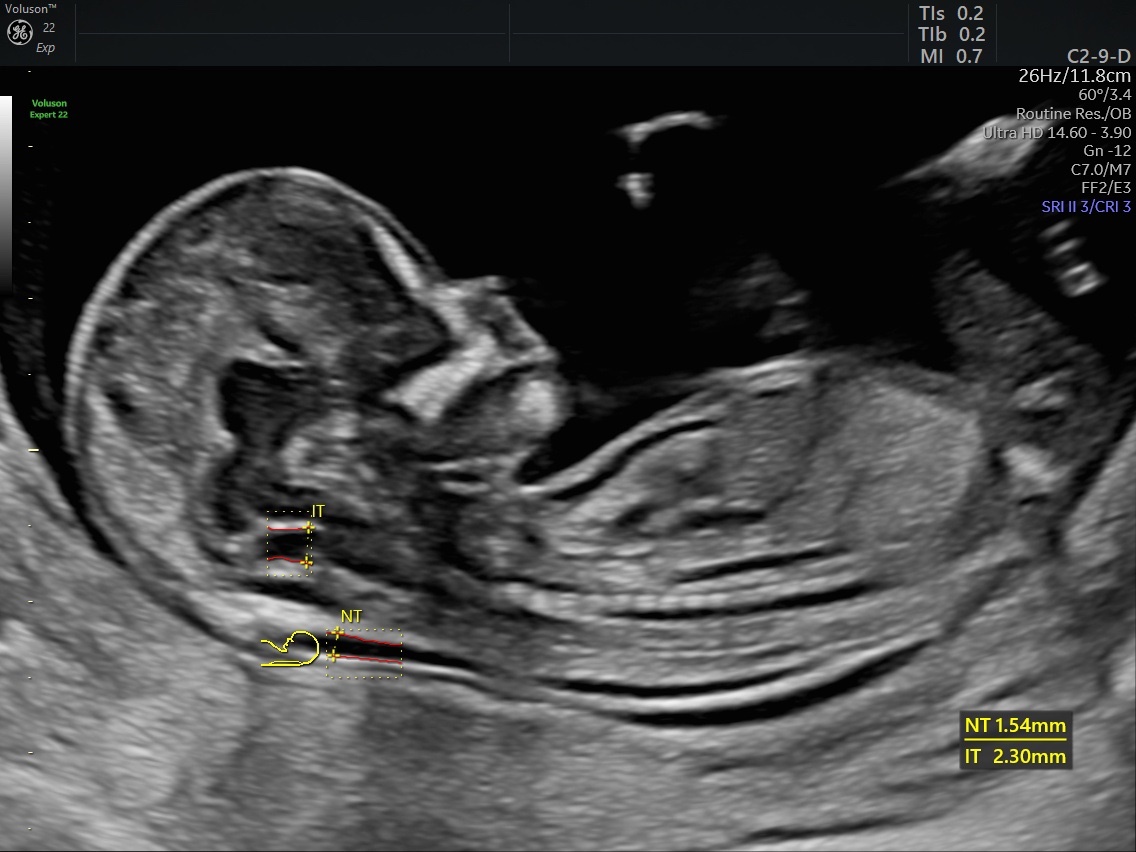
Measure nuchal and intracranial translucencies with the automation tool SonoNT™/SonoIT – (Sonography-based Nuchal/Intracranial Translucency), Voluson™.
An inside-to-inside measurement in an appropriately sized photo featuring the fetal head in midsagittal view with the nasal bone is essential. This region is incredibly small, and therefore, precision is critical. Even a slight incorrect measurement might lead to a false-positive "abnormal" result and a series of unnecessary investigations.
The ultrasound test for fetal nuchal translucency aims to predict chromosome abnormalities, specifically trisomy 21 (Down syndrome), trisomy 12 and trisomy 18. In addition, an NT measurement above the threshold of normal may indicate the presence of physical abnormalities, such as a fetal heart defect.
What a Patient Can Expect During an NT Ultrasound
During pregnancy, ultrasounds can be performed transabdominally or transvaginally. In general, transabdominal ultrasound is the go-to option during pregnancy, but for early pregnancy indications, including an NT ultrasound, a supplemental transvaginal ultrasound can be helpful. The ultrasound test for fetal NT must be performed during a specific window: between 11 weeks and 5 days and 13 weeks and 6 days of gestation. A patient should attempt to use a reliable last menstrual period or early pregnancy dating ultrasound to date the pregnancy with enough notice to schedule an NT ultrasound during this time frame.
If the booking is made before the 11 weeks and 5 days cut-off, it simply requires a rescheduled appointment. On the other hand, if the ultrasound test for NT is scheduled after 13 weeks and 6 days gestational age, the window is missed and the NT becomes unreliable.
If the patient is interested in risk assessment for chromosomal anomalies, they would book the ultrasound test for fetal NT and the associated bloodwork. Both the NT and bloodwork markers are part of the parameters used for the enhanced first-trimester screening tests (eFTS). In other words, the NT measurement is combined with blood test results to assess the likelihood of trisomy 21 or trisomy 18. Many expectant parents decide to undergo this genetic testing, including the NT, for preparedness sake and to ensure the fetus is in good health. A stand-alone NT ultrasound is recommended for twin pregnancies, as the eFTS cannot be performed due to unreliability.
Patients should be aware that a referral is needed for the ultrasound test from a general practitioner or OB/GYN in most jurisdictions.
Biomarkers Used in Enhanced First-Trimester Screening Tests
Several bloodwork biomarkers are used to help determine normal vs. abnormal results in eFTS. According to Prenatal Screening Ontario, the levels of three or four different hormones and proteins will be measured by taking a blood sample:
- Pregnancy-associated plasma protein A, a protein made by the placenta
- Human chorionic gonadotropin, a hormone made by the placenta during pregnancy
- Alpha-fetoprotein, a protein made by the baby's liver
- Placental growth factor, a protein made by the placenta
It is the results of these blood tests and the NT measurement combined that provide a final result. The results of eFTS will usually return as "screen positive" or "screen negative." When the result is abnormal — "screen positive" — further testing can be performed if desired by the patient. Occasionally, a screen positive result is not followed by a positive confirmatory test. The false positive rate for eFTS for trisomy 21 is 6%. For trisomy 18, the false positive rate is less than 1%. On the other hand, screening cannot perfectly detect trisomy 21 and 18 in every patient. eFTS correctly picks up 89% of trisomy 21 and 85% of trisomy 18, missing the remainder.
Regardless of the "screen negative" or "screen positive" result, patients will receive a specific risk of trisomy 21 (for example, a result may be a 1 in 24 or 1 in 900 chance that the baby has trisomy 21).
Next Steps for Patients and Providers
Once a patient's results are determined, following through with next steps is pivotal — especially when the eFTS or standalone NT (in the context of twins, for example) is abnormal. The other more accurate option that can be offered after a screen negative eFTS is noninvasive prenatal testing (NIPT). This relatively novel blood test is not covered by every health system for every patient automatically. Although patients who are not covered for this test may decide to pay out of pocket for it (and can do so earlier in gestation as early as nine weeks), patients with abnormal eFTS will usually be able to access NIPT.
Alternatively, diagnostic tests such as chorionic villus sampling or amniocentesis can be performed and provide patients with the diagnostic clarity of a "yes" or "no" answer about both trisomy 21 and 18 during the pregnancy. Chorionic villus sampling needs to be done between 11 and 14 weeks. This can be logistically difficult if the NT and eFTS are completed into the 13-week gestational age period. Conversely, amniocentesis needs to be performed after 15 week gestation. Amniocentesis is generally preferred for diagnostic certainty in abnormal eFTS.
Patients should opt for further ultrasounds for the evaluation of anatomy as the pregnancy develops. Traditionally, anatomy or morphology scans would be performed between 18 and 20 weeks. Many centers are pushing the envelope and assessing detailed anatomy earlier in gestation. Regardless of when it is done or what the previous result of eFTS/NT was, this information is also critical to the prospective parent(s).
Looking Toward the Future
The ultrasound test for fetal NT has been around for a long time. However, research is still being done to evaluate its utility, particularly against other screening methods, as research from the journal Prenatal Diagnosis reports. Although exciting alternatives are being developed, NT still has significant value. One study published in the American Journal of Obstetrics and Gynecology decided to challenge the approach of capturing the NT on ultrasound, evaluating the transverse view of the NT, rather than the classic sagittal view. Interestingly, the authors found that if the scan was performed by an expert sonologist, there was only a minimal difference in NT measurement between the two planes, sagittal and transverse. This may mean an NT assessment on transverse views could be within the realm of possibility; although for now, it would still not be preferable. This may be most relevant if the sagittal views are difficult to capture and transverse views are easier.
Although new techniques for prenatal screening and diagnosis are being studied every day, the NT has stood the test of time. It is essential that healthcare providers and patients alike understand the utility of this test, its strengths and limitations, and the logistics. As a safe, simple and affordable test, the ultrasound test for fetal NT is likely to continue to be a major player in the identification of chromosomal and anatomical anomalies.