Pelvic inflammatory disease (PID) is, for the most part, a "social disease" that flourishes when introduced to the sexually active teenager, the divorcee just starting to date again or even the happily married woman. All are at risk. Less than 15 percent of acute PID is caused by enteric bacteria or respiratory pathogens that colonize the pelvic region and the upper genital tract of women. The majority of PID cases are due to exposure to a sexually transmitted infection (STI).
Pelvic inflammatory disease and STIs create a significant burden to the patient and the health system, which is why PID prevention is important. The Centers for Disease Control and Prevention (CDC) estimated that nearly 20 million new infections happen in the U.S. each year, costing the healthcare system nearly $16 billion in direct medical costs alone. Almost half of those affected are under the age of 25.
An increase in STIs for four consecutive years was reported at the recent National STD Prevention Conference in Washington, D.C. Chlamydia remains the most common STI disclosed to the CDC. Left untreated, PID increases the risk of infertility, ectopic pregnancy, stillbirth in infants, chronic pelvic pain and even elevated HIV risk.
PID Prevention Is Key
Prevention is the best solution. Abstinence and barrier contraceptives have a significant role in reducing exposure and preventing STIs and PIDs. Male and female condoms offer protection from STIs, with both latex or synthetic male condoms offering the best defense. Natural membrane condoms made from lamb cecum are porous, which may allow passage of viruses, including HIV, hepatitis B and the herpes simplex virus. Latex and synthetic male condoms offer protection not only against viruses but skin-to-skin transmission of HPV, chancre, syphilis and chancroid as well.
Routine screening and early recognition and treatment of symptoms are key. Any woman of reproductive age presenting with pelvic pain should be checked for STIs. Doctors should initiate antibiotic treatment if PID is high on the differential list — even if testing or results are not available. Overtreatment is not a concern, but a delay in treatment is. Even waiting a few days increases the risk of long-term sequelae, including infertility.
The complete checkup should include abdominal, speculum and bimanual exams with the collection of appropriate tests for STIs, urine and blood work. Ultimately, this is a clinical diagnosis. The differential includes appendicitis, ectopic pregnancy, ovarian torsion, intrapelvic bleeding, rupture of an adnexal mass, endometriosis and gastroenteritis.
Treating PID and STIs
Transvaginal ultrasonography has a long history as the go-to imaging tool to identify and evaluate those requiring treatment for suspected PID. An article in Obstetrics and Gynecology from 1992 determined that the finding of thickened fluid-filled fallopian tubes has an 85 percent sensitivity and 100 percent specificity for endometritis. In 1998, Timor-Tritsch, et al., described the ultrasound findings of acute and chronic salpingitis. Tube dilation, shape, wall thickness and the presence of free pelvic peritoneal fluid were considered. The presence of a partial septum of the tubal wall was noted to be pathognomonic for both acute and chronic PID. Acute salpingitis appeared on ultrasound most often as thickened, hyperemic tubal walls with a cogwheel appearance, while thin tubal walls with "beads-on-a-string" indicated chronic salpingitis. A follow-up ultrasound in six to eight weeks to document stability or resolution of salpingitis is highly recommended.
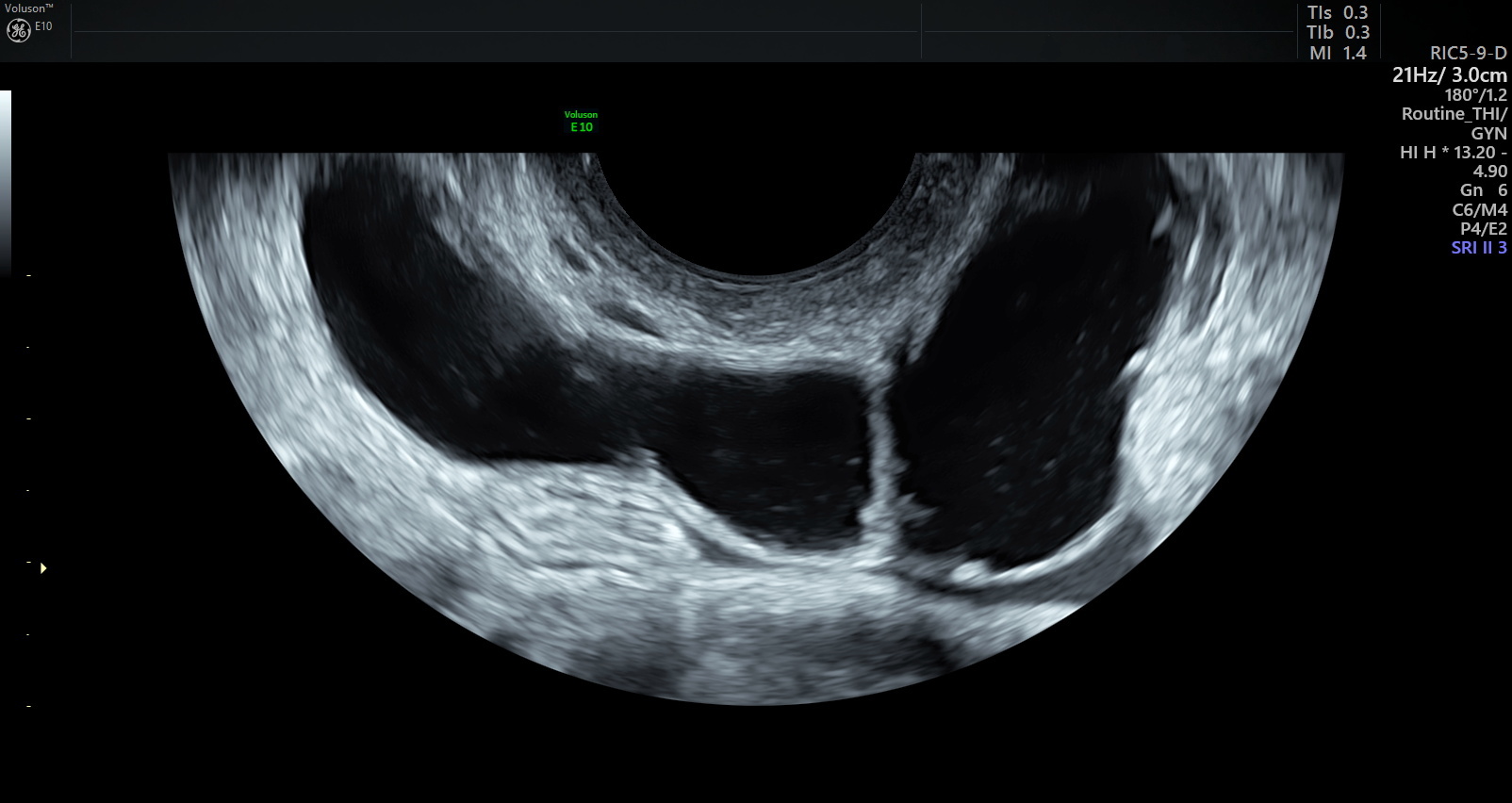
Transvaginal ultrasound image of dilated fallopian tube
Tubo-ovarian abscesses (TOA) occur in about one-third of women with PID. Ultrasound findings of a TOA include thick-walled, dilated tubes and complex adnexal masses with irregular margins. When evaluating abnormal findings on transvaginal ultrasound in the setting of PID and TOA, 3D ultrasound has been especially helpful. It is significantly cheaper than MRI and also more readily available in the outpatient setting. Of course, if TOA is suspected, in-hospital treatment is needed.
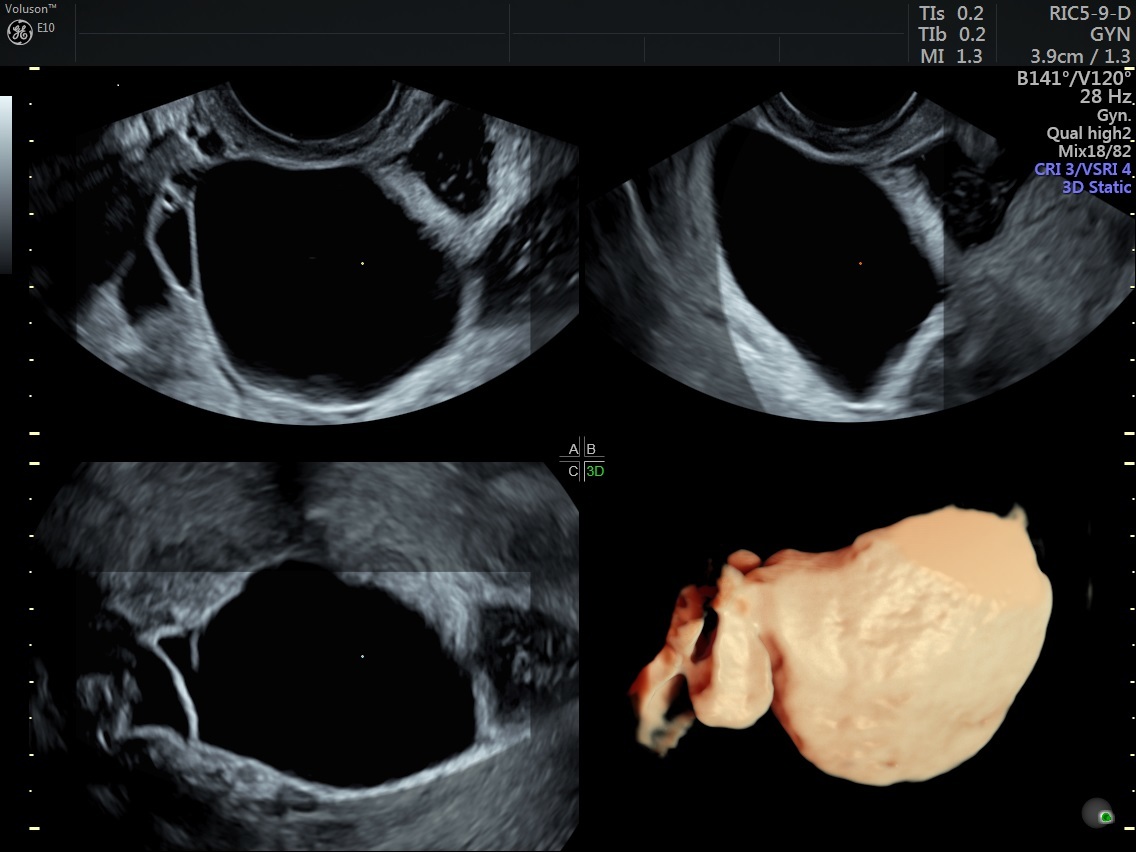
3D ultrasound of fluid-filled fallopian tube
"Social disease" may be a euphemism for venereal disease, and PID can certainly be a consequence of it. But, unlike some of the other problems we may face, PID is preventable and treatable.



