The "G3P1Ab2" marked on Gloria's chart reveals her complex reproductive medical history: three pregnancies, one live birth and two abortions. This 36-year-old mom presents as a work-in for an urgent office appointment one morning when she starts experiencing persistent vaginal bleeding. It begins 3 weeks after what she thought was a spontaneous miscarriage, with the passage of tissue at home at approximately 10 weeks gestational age.
In the 48 hours leading up to her appointment, Gloria has noticed an increase in the bleeding, and she has passed several clots. She reports moderate cramping in the lower pelvis bilaterally that has not responded to over-the-counter NSAIDs. She is currently saturating a pad every 2 hours but denies syncope, palpitations, shortness of breath or fever. She also denies experiencing any GI symptoms or hyperemesis. Her past obstetrical history is notable for an uncomplicated dilatation and evacuation in the first trimester of a molar pregnancy followed by a term pregnancy with a scheduled cesarean section delivery for breech presentation.
Initial Exam and Findings
On examination, Gloria appears to be in moderate pain. Her vital signs are stable without evidence of orthostasis. She is afebrile, her abdomen is nondistended and there is no rebound. Brisk bleeding is encountered on the pelvic exam. Small clots are evacuated in order to clearly visualize the cervix. No lacerations are identified. No tissue is noted and the cervix appears dilated. There is no cervical motion tenderness, and the 8-week-size uterus is minimally tender. The left adnexa, however, is moderately tender.
A urine pregnancy test is negative. A fingerstick hemoglobin is 11 g/dl. Blood is drawn and sent to the lab for a human chorionic gonadotropin (hCG) assay, a blood type and Rh, complete blood count (CBC) with differential, comprehensive metabolic panel (CMP), coagulation studies and lactic acid. The physician has these tests expedited.
Ultrasound Findings
In the meantime, Gloria's gynecologist performs an ultrasound. The transabdominal scan reveals no large pelvic masses. The uterus is retroverted. The endometrium appears thickened, measuring 10 mm. Fluid is noted in the pouch of Douglas. A peristalsing bowel with gas limits the transabdominal view of the adnexa.
On transvaginal ultrasound, the uterine measurements are at the upper limits of uterine size: 9.4 x 5.7 x 6.9 cm. No gestational sac is seen. However, a heterogeneous echogenic mass of 2.5 cm at its greatest diameter is seen in the endometrial cavity at the fundus. It is measured in three dimensions and 3D images are obtained.
The fundal myometrium appears normal. The endometrial-myometrial junction appears smooth. Color Doppler confirms the presence of a fundal feeding vessel and flow within the mass, with a peak systolic flow of 40 cm/s. The adnexa are visualized and measure within normal size. The right ovary measures within normal limits. There is a thick-walled cyst with a fine internal lace-like pattern on the left ovary measuring 1.7 cm at its greatest diameter. Gloria reports some tenderness while the left adnexa is evaluated sonographically. The fluid in the pouch of Douglas is noted to be minimal.
The Diagnosis: Retained Products of Conception
When Gloria's gynecologist reviews the findings with her, they give her the differential diagnosis of retained products of conception (RPOC) versus an endometrial polyp. Gloria and her doctor discuss the risk and benefits of medical versus surgical treatment, and Gloria elects to proceed with hysteroscopic removal of the tissue. The gynecologist tells her that this choice ensures complete removal and may reduce the formation of intrauterine adhesions when compared to a blind procedure.
Next, the gynecologist alerts the surgical team and obtains Gloria's informed consent. In the meantime, some of the labs have returned: Bloodwork shows no evidence of infection or coagulopathy. Gloria is transferred to the procedure room and agrees to undergo surgery that same afternoon. An intraoperative transabdominal ultrasound confirms the mass has been removed in its entirety, and the tissue is sent to pathology for permanent sections.
How Early Pregnancy Loss Leads to RPOC
Early pregnancy loss occurs in about 15 percent of registered pregnancies, but the rate may be as high as 31 percent, according to research published in the British Medical Journal. The risk of miscarriage rises with advancing maternal age and previous history of pregnancy loss. Hemorrhage is a common complication of early pregnancy loss and when bleeding occurs several weeks out from the passage of tissue, this is suggestive of RPOC.
To differentiate RPOC from a blood clot, the presence of vascularity is helpful in clinching the diagnosis — although as RPOC are reabsorbed they lose their vascularity. This means that the absence of flow does not necessarily rule out RPOC. Saline infusion sonography may be considered if the diagnosis is unclear, the patient is not bleeding heavily and there are no signs of infection. Endometrial thickness has also been evaluated as a possible predictor of RPOC but has not been found to have a high predictive value, according to research published in Ultrasound in Obstetrics and Gynecology.
Considering Placenta Accreta
Retention of placental tissue or fetal tissue in the uterus after pregnancy might occur after a spontaneous miscarriage, a planned elective termination or a delivery. It can also be a cause of postpartum hemorrhage. When it occurs after cesarean delivery, abnormal placentation such as placenta accreta should be considered. Placenta accreta has also been reported in early pregnancy. According to a study published in Obstetrics and Gynecology Science, if this condition is not ruled out, it can lead to catastrophic bleeding at the time of dilation and curettage (D and C) for RPOC.
Gloria had several risk factors for a placenta accreta, including advanced maternal age, a history of a previous D and C, and a history of a cesarean section. A high level of suspicion on the clinician's part and careful ultrasound evaluation of the myometrium will help reduce the likelihood of missing this important diagnosis. Some clinicians feel the presence of vascularity in the RPOC and the size of the remaining RPOC are both markers for increased failure to respond to treatment. Endometritis, sepsis, coagulopathy and toxic shock are potential complications of RPOC and should factor into management decisions.
Gloria's history of a previous molar pregnancy raises concern for the diagnosis of another molar pregnancy — but with a negative urine hCG, it would be unusual. Ruptured ovarian cyst and ectopic pregnancy are also possible causes of her symptoms but are readily ruled out once the ultrasound is performed.
Endometrial polyps have been associated with infertility and pregnancy loss. They can occur at any time in a patient's reproductive life. They are usually benign and asymptomatic but can present as abnormal vaginal bleeding. CT and MRI are not necessary for diagnosis.
On follow-up 4 weeks later, Gloria reports no complications from the procedure and no further bleeding. Her pelvic exam is normal. An ultrasound shows the resolution of the left ovarian cyst and a dominant follicle on the right ovary. The endometrium appears smooth and without evidence of masses or adhesions. The physician advises Gloria that the final pathology confirms chorionic villi, verifying the diagnosis of RPOC.
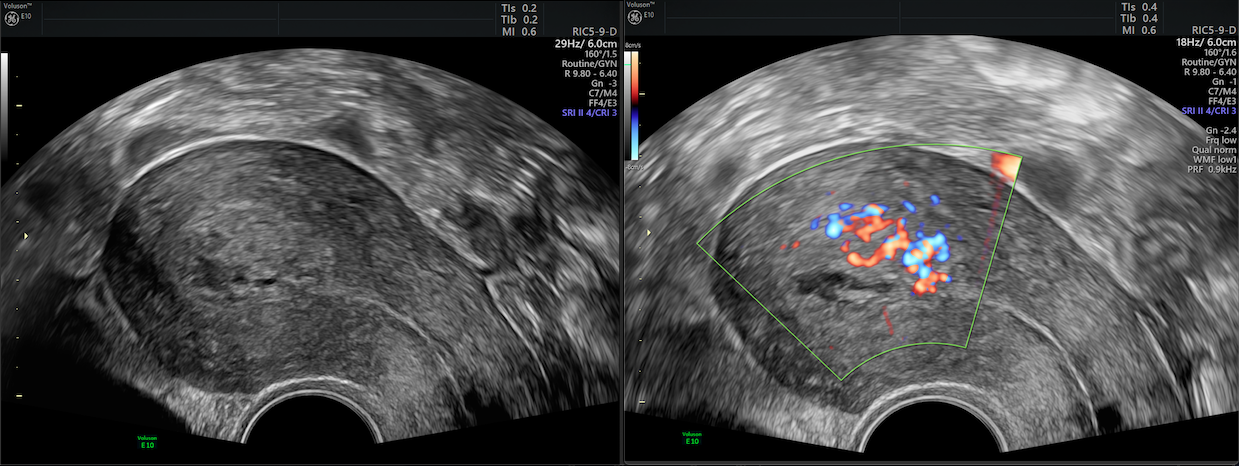
Retained products of conception, 2D demonstrates heterogeneous echogenic mass and color Doppler, fundal feeding vessel with flow in mass



