Many women experience some loss of bladder control during their lives, and the frequency of this increases with age. Yet far too many of them don't report urinary incontinence to their doctors. Understanding why women are hesitant to talk about such a common problem can help doctors find ways to broach the subject with patients and offer assistance.
Older Women and Urinary Incontinence
A recent University of Michigan National Poll on Healthy Aging found that 46% of women ages 50-80 experienced urinary incontinence, with 41% of them describing the symptoms as problematic. "Problematic" is a sign that this issue is lowering the patient's quality of life.
Most women in the poll said they experience leakage when they sneeze or cough, when trying to get to the bathroom or when exercising. Despite the frequency or discomfort of this loss of bladder control, only 28% of women ages 50-64 said they talked about incontinence with their doctor.
Why Women Aren't Speaking Up About Loss of Bladder Control
Loss of bladder control is a pretty common occurrence after childbirth. Many young moms even joke about leaking every now and then, assuming it's normal.
Part of the reluctance may be because women assume it's a common part of aging or a normal side effect of having kids. There's no point in talking about it, many think, because it happens to everyone.
Shame and embarrassment can contribute to silence as well. This may be generational, as older women may be less willing to openly discuss bladder leakage than their younger counterparts.
But treatment for urinary incontinence in elderly female patients may be limited if they don't talk about it. A survey by the National Association for Continence (NAFC), which featured mostly respondents over age 65, found that about 20% of patients felt their concerns weren't taken seriously by their doctor.
Another NAFC survey found that 80% of respondents frequently dealt with incontinence, yet 50% of them felt uncomfortable even talking to friends and family about it.
How to Broach the Subject of Urinary Incontinence
You may have some patients who are more reluctant to discuss loss of bladder control than others, but it's best to ask everyone. Let your patients know that it's normal and may be caused by childbirth or even hormonal changes. Even if your patient isn't experiencing incontinence now or doesn't feel comfortable talking about it yet, asking the question can open the door for a future conversation.
When broaching the subject, let your patients know there are painless ways to diagnose and treat the condition. First, you need to know their symptoms to uncover what type of incontinence they have; encourage them to keep a log at home of incontinence instances. Then, a urinary incontinence diagnosis can be made by reviewing this log, conducting a urine test and doing an ultrasound.
A common test involves using 3D ultrasound to measure post-void residual volume. Explain to patients that you'll use the ultrasound to measure bladder volumes before and after urinating to get a better sense of what's happening. Most gynecology patients are already familiar with ultrasounds, making the diagnostic process less intimidating. The fact that the procedure is quick and minimally invasive should help ease their concerns further. Using an ultrasound to examine the pelvic floor also helps detect injuries, tears or abnormalities and can inform any surgical approach.
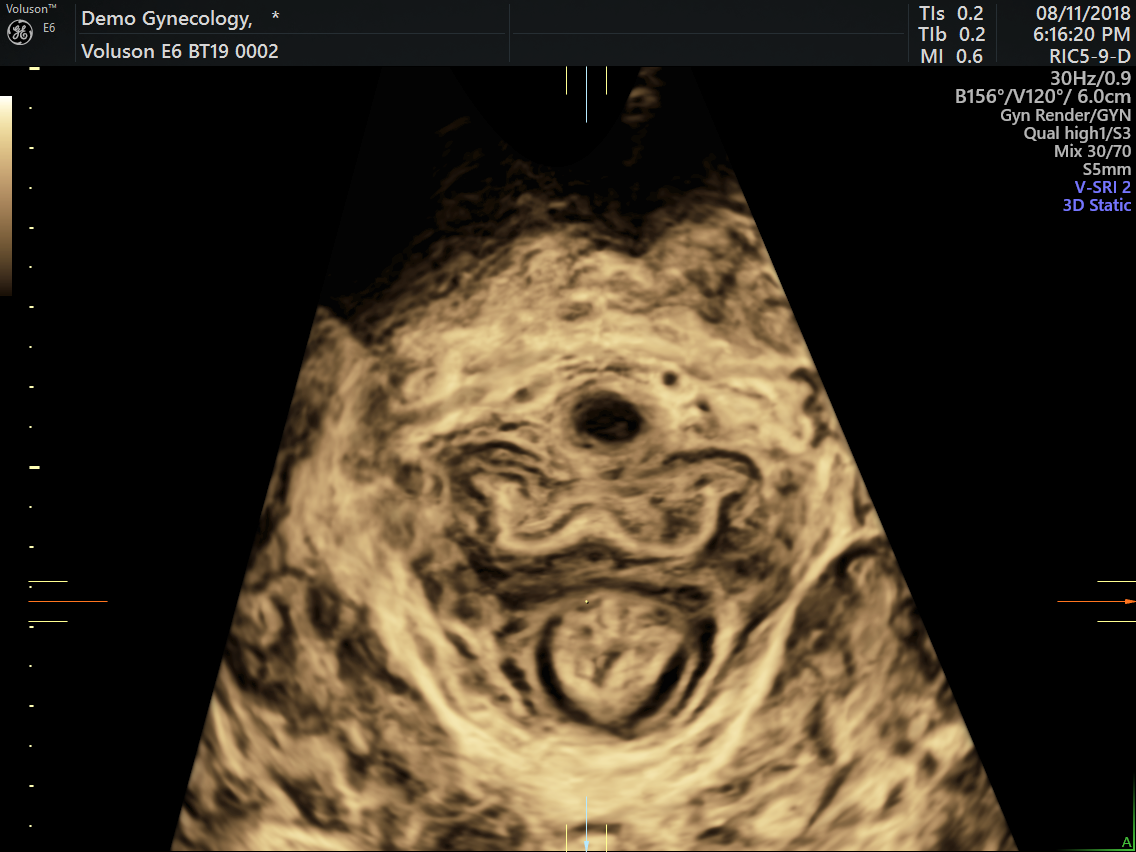
3D ultrasound of pelvic floor
3D ultrasound visualizes the pelvic floor to help uncover the cause of urinary incontinence.
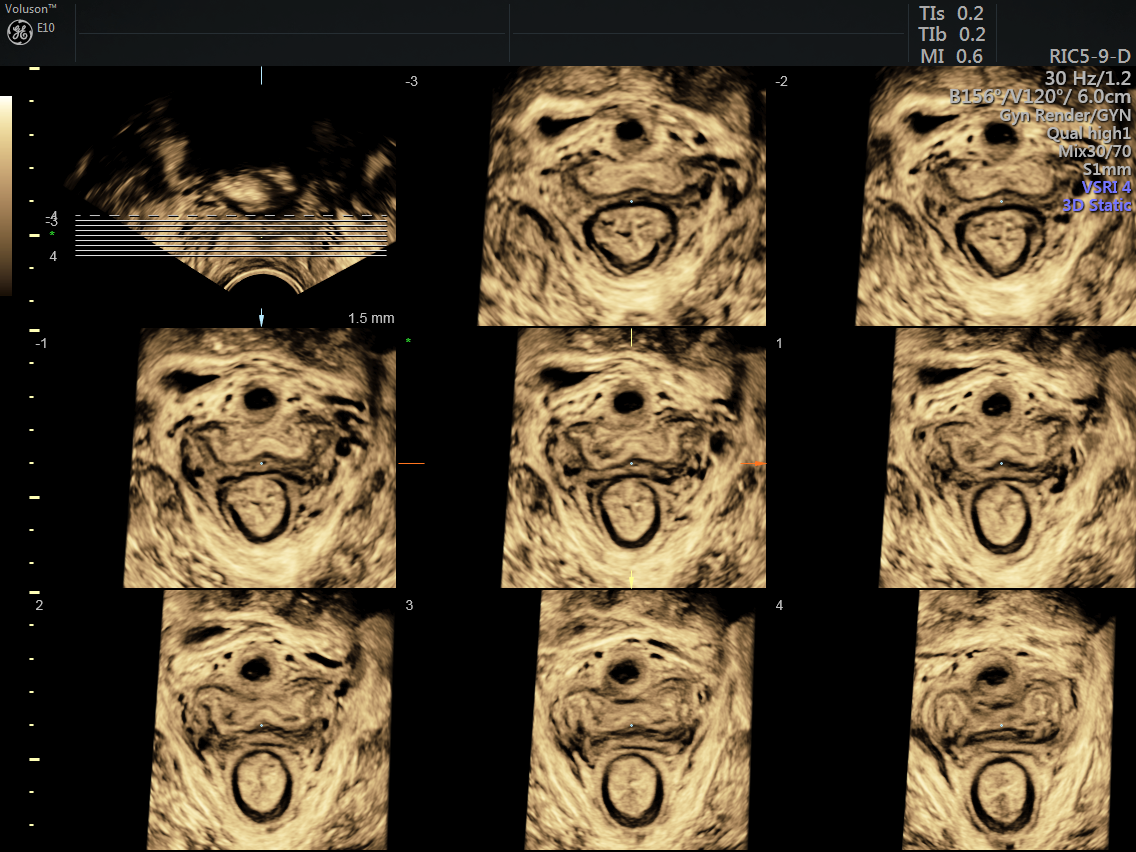
Pelvic floor 3D ultrasound with TUI
3D tomographic ultrasound imaging (TUI) of the pelvic floor provide parallel slice of a dataset for even more visualization.
Talking to Patients About Options
Doctors should educate patients about treatment options, too. Reassure them that you have many non-invasive, at-home options to manage loss of bladder control. Dietary modifications, behavior training and pelvic floor exercises are a first step for mild symptoms. Medications, electrical stimulation or devices may be needed if the problem continues or is more severe. Surgery is also an option if other treatments haven't worked and the urinary incontinence is having a detrimental effect on quality of life.
Starting the conversation and ensuring patients are properly educated about incontinence are the first steps to improved outcomes. Reassure patients that incontinence isn't just a part of aging they have to deal with — there are ways to manage it.



